When Do I Bring My Child for a Speech Sound Evaluation?
As our children grow and develop speech, they don’t learn to use all the speech sounds in their native language simultaneously. That’s why my little one tells me that “it’s dart outside” when he looks out the window after dinner these days! But how do you know when to seek out a speech therapist for your child?
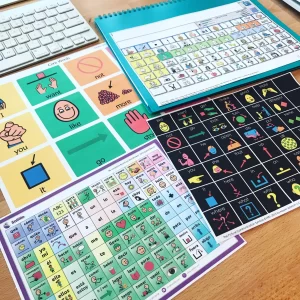
Check out the chart below, which is available as a downloadable PDF on the SLP now website at https://blog.slpnow.com/the-slps-guide-to-speech-sound-disorders-articulation-phonological-development/; when looking at the chart, understand that some children start to develop sounds before the ages listed. The ages listed represent the age at which 90% of children have mastered each sound. For many speech sounds, there is a wide range of ages at which a child may start to produce the sound or approximations inconsistently before they truly master the sound. However, it is a quick rule of thumb that if a child cannot produce one of the sounds listed under their age, speech therapy may be indicated.

What Can I Do at Home to Help My Child with Their Speech Sounds?
So, what can a parent do to help their child develop speech sounds correctly at home? The first strategy I recommend is to make sure your child is looking at your face when you’re producing words or sounds that they had difficulty with. Draw attention to your mouth by pointing. Children learn a lot about how a sound is produced by observing you.
Another strategy that you can use is called recasting. Recasting is when you repeat what your child says precisely, including the errors, in a questioning voice. For example, if your child says, “Look at the tar” when they mean “Look at the car,” you might respond by saying, “Tar? Is that what you meant?” When the child attempts to correct himself or herself, if he or she cannot do so, I suggest using the first strategy we discussed. Your child may not produce the sound at that moment, but that’s okay because they are still learning from what they see and hear from you.
I also recommend reading with your child regularly. Even if a child cannot read independently, draw their attention to some of the letters in the book, especially if the book has large decorative letters at the beginning of paragraphs. Talk about the sound the letters make, and again, ensure your child is watching your face.
For emerging readers, phonics activities are an excellent time to work on articulation at home. While doing phonics homework with your child, could you talk about how each sound is made? For example, the “T sound is made with our tongue on the roof of her mouth.” If you’re unsure how to describe how sounds are made, PeechieSpeechie.com has an excellent video library with tutorials for each sound.
If your child is receiving speech therapy services, their SLP will be able to provide you with additional, personalized resources.
How Can Carolina Therapy Connection Help?
If you are still unsure or feel that your child’s speech is difficult to understand compared to others his/her age, Carolina Therapy Connection has licensed Speech Language Pathologists at the clinics in Greenville, Goldsboro, and New Bern that are highly qualified to evaluate and diagnose speech sound disorders. You can schedule a speech sound evaluation at whichever clinic is most convenient for your family at 252-341-9944. Our professionals can also provide personalized resources for your child’s needs.
By Michelle Berghold