What are Some Winter Activities When the Weather is too Cold Outside?
Ever wonder what you can do to keep your Kiddo occupied and safe while providing the necessary sensory input when it’s too cold to play outside? It is recommended to take indoor breaks every 20-30 minutes when the temperature outside is between 13-30 degrees; however, some kiddos tolerate cold weather better than others. Here are some tips for activities that can be done indoors when it’s just too cold to go outside this winter!
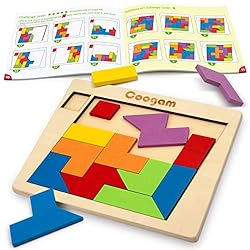
A Fun Winter Activity: Play Board Games
This is dependent on your child’s age and skill set. If you have some board games tucked in the closet, break them out and have family fun! This will work on building your child’s reciprocal play skills, following multistep direction skills, coping skills, and emotional regulation. Check out our Amazon storefront for some of our recommended board games!
Build a Pillow/Blanket Fort
Who didn’t love making a fort under the kitchen table as a kid? Build a fort in the kitchen and living room, then place some of their favorite books, toys, and stuffed animals inside. This can be a fun way to get your kids into critical thinking mode and build their visual perceptual and motor skills!

Scavenger Hunt
Another fun winter activity is to hide some items in your house and have your kiddos find them! This can be graded according to skill level and age. For example, for a younger kiddo, have them locate items they would typically use. For older kiddos, give hints to the item they are looking for. “Find two things mom uses to stir within the kitchen (utensils)” or “Find something round and blue in your bedroom (ball).” This will work on their figure ground skills and get their body moving!
Bake/Cook
Have your kiddos help you bake/cook your favorite snack or dessert in the kitchen. Have your kiddos follow the directions given or help with the messy tasks. This can be great for our sensory-seeking kiddos and those resistant to messy play!
Dance Off!
GET MOVING with a fun dance-off! Put off some of your favorite music and have a contest to see who dances best to the song! This is a great way to work on gross motor skills, coordination, and auditory processing, and it’s just plain fun!
Watch your Favorite Movie and Act Out the Scenes.
Many kids like to watch movies; however, do you ever notice that they get bored halfway through and are on to the next thing? Get them involved with the movie. Have that pause button ready and have them act out a scene to see if they can recall what happened!
Indoor “Snowball” Fight
Do you have some extra tissue paper lying around after wrapping those Christmas presents? Make snowballs and toss them at each other! This is a great way to get kiddos moving without fear of knocking things off tables/counters and breaking things!
Keepie-uppie with Balloons
Everyone knows this one! Can we keep the balloon off of the ground? Try it! It is so much fun, works on your kiddo’s hand-eye coordination, and has less risk of damaging something in your home!
How can Carolina Therapy Help?
With winter in full swing, ask your therapist about tips/tricks to have fun indoors with adaptations specifically for your child’s sensory-related needs. A therapist at Carolina Therapy Connection can help adapt the activities listed above and give more ideas for your specific child! Also, check out our link for Amazon storefront to find fun toys/activities to make the indoors fun! Many great toy ideas and sensory-related tools can be used when your child needs to get some energy out!
I hope these tips have helped build some fun ideas for you and your family for this winter season! Stay happy, healthy, and warm!
By: Shelby Godwin, COTA/L, AC